October 22, 2024, 9:40 am | Read time: 5 minutes
Rhinosinusitis is the word par excellence for the cold season: sinusitis. Almost everyone has sniffled or struggled for breath because of it. Read on to find out how the disease progresses, why decongestant nose drops are the wrong treatment, and which non-medicinal methods are useful instead.
A runny nose and a sore head: in the fall, sinusitis threatens again. Sinusitis is what the experts call it. Or even rhinosinusitis. This is what Prof. Martin Wagenmann, Head of the Rhinology, Allergology, and Endoscopic Skull Base Surgery Department at Düsseldorf University Hospital, talks about. This is because the nose itself is usually also affected. “There are very few people who never have sinusitis in their lives,” Wagenmann tells FITBOOK. Here, you can read about the symptoms of sinusitis, whether decongestant nasal drops help, the benefits of antibiotics, and when surgery makes sense – as well as which non-medicinal therapies can help.
Overview
Acute and chronic rhinosinusitis
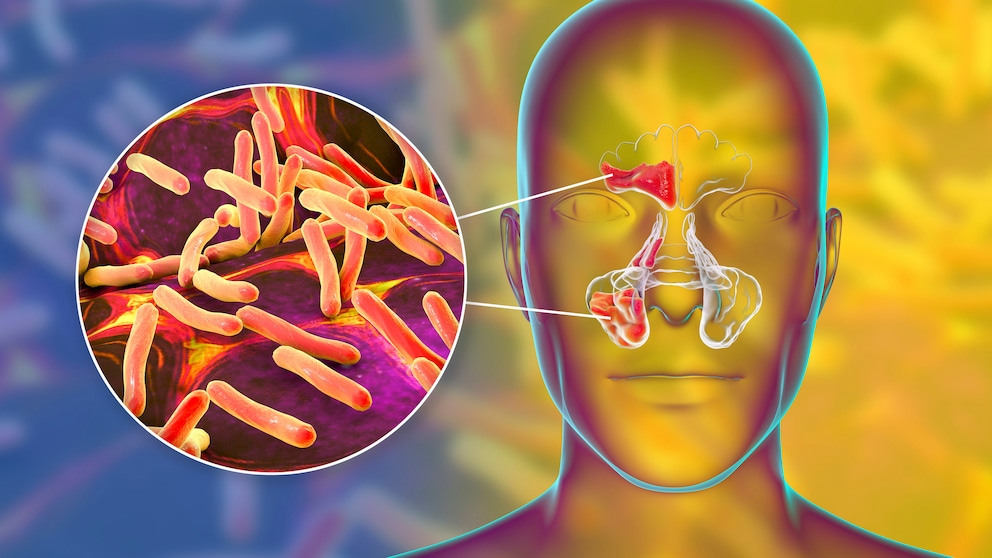
A distinction is made between two forms, as the expert from the German Society for Ear, Nose and Throat Medicine, Head and Neck Surgery explains to FITBOOK: acute rhinosinusitis (acute RS or ARS for short), which can last up to three months, and chronic rhinosinusitis (chronic RS, also known as CRS). Acute sinusitis is triggered by viruses or, more rarely, bacteria. This causes nasal secretions to be produced en masse, a mixture of fluid, proteins, and fats.
Course of rhinosinusitis
In 60 to 80 percent of those suffering from acute RS, complete healing occurs within two weeks without therapy. 90 percent recover within six weeks.
Chronic RS is sometimes associated with a course that can last for years or even a lifetime.
Typical symptoms of sinusitis
Typical complaints and symptoms of sinusitis are
- Nasal obstruction
- Secretion runs out of the nose and/or backward into the throat (anterior or posterior secretion)
- Facial pain
- Disturbance of smell
- Optional complaints or symptoms (fever, headache)
What helps with sinusitis?
The treatment of sinusitis depends on whether it is acute or chronic and whether it is caused by viruses or bacteria. First, a high fluid intake (water, tea) ensures that the mucus becomes thinner and can drain more easily. What also helps with sinusitis is sufficient rest and sleep to support the immune system.
Can decongestant nasal drops speed up the recovery process?
Decongestant nose drops do alleviate the symptoms … “but you shouldn’t think that you can accelerate the course of the disease with them,” explains the doctor when asked by FITBOOK.
Hype about decongestant nasal drops and the risk of addiction: Nevertheless, Germans are world champions when it comes to buying decongestant nasal drops. According to the German Medical Association, the ten best-selling over-the-counter medicines in 2019 included preparations containing the nasal spray active ingredient xylometazoline in 1st, 5th, 7th, and 8th place – a total of 59.5 million packs sold. In 1972, only 7.4 million packs were sold in West Germany.1 Addiction to nasal sprays is now a major issue.
What are the benefits of antibiotics?
From Wagenmann’s point of view, treatment with antibiotics is usually not advisable. “Over 90 percent of inflammations are not caused by bacteria.”
Which non-medication treatment methods are effective?
For acute rhinosinusitis, the S2k guideline Rhinosinusitis of the German Society for Ear, Nose and Throat Medicine, Head and Neck Surgery recommends local applications with saline solution, for example as nasal drops or spray, as well as inhalation of hot vapors (38 to 42 degrees Celsius). Therefore, the nasal application of saline solutions should be used for the symptomatic treatment of chronic rhinosinusitis.
The effectiveness of acupuncture and homeopathy cannot be conclusively assessed due to the limited data available.2
When is surgery recommended?
Does surgery help with sinusitis? According to Wagenmann, around eleven percent of the population in Europe is affected by chronic rhinosinusitis. “This can then restrict the quality of life in a similar way to asthma,” he tells FITBOOK. If drug treatment does not help, surgery can be useful. This involves widening the openings to the nose.
According to hospital statistics from the Federal Statistical Office, over 450,000 operations were performed on the nose and sinuses in 2018.3 “In the past, too much mucous membrane was removed. Today we know that these radical operations usually do more harm than good,” says Wagenmann. Nevertheless, too many surgeries are probably performed – which is due to the fact that operations are lucrative in our healthcare system.

Also Known as Coneflower Taking Echinacea Correctly — When the Medicinal Plant Can Help

Currently rising figures Symptoms that may indicate a mycoplasma infection

Holistic healing method Who osteopathy is suitable for and how treatment works
Why do we have sinuses at all?
From a purely anatomical point of view, sinuses are air-filled outpouchings of the mucous membrane in the nasal cavity. Doctors distinguish between four different ones in humans: the maxillary sinus, the frontal sinus, and the sphenoid sinus, as well as the ethmoid cells located between them. But why do humans have sinuses in the first place?
“Nobody knows exactly, the evolutionary function is still unclear,” Wagenmann tells FITBOOK. One theory is about resonance for a richer-sounding voice. Another is a built-in crumple zone. “In a collision with a mammoth, it was better for the face to be compressed than for the base of the skull to be fractured.”
“The sinuses have nothing to do with smelling or breathing”
Reduced weight might also be a factor: Air is lighter than bone. In addition, the concentration of nitric oxide in the sinuses is high – and this has an antibacterial effect, says Wagenmann. “Only one thing is certain: the sinuses have nothing to do with smelling or breathing,” he explains. “The openings to the nose are far too small for this to have any effect.”